Eye care professionals consistently strive to enhance their diagnostic capabilities to provide optimal vision health for their patients. One crucial tool in their arsenal is the Esterman visual field test, a well-established and reliable method for evaluating peripheral vision. The Esterman visual field test, which is used in many states to determine driving eligibility and assess binocular peripheral vision, is a 120-point suprathreshold exam required by DMVs and licensing boards. Eye doctors rely on the Esterman visual field test to quickly evaluate functional peripheral vision and document impairment for glaucoma, retinal disease, and neurological conditions.
Beyond central vision, a healthy peripheral field allows for crucial tasks like safe driving, obstacle avoidance, and spatial awareness. Detecting early peripheral vision loss can aid in diagnosing and managing various eye diseases before they significantly impact central vision and daily life – the Esterman exam helps with that detection.
This article provides eye doctors and healthcare professionals with a detailed understanding of the Esterman test, including its purpose, methodology, applications, advantages and limitations.
What Is the Esterman Visual Field Test?
The Esterman is a wide field of view exam that tests the outer edges of a patient’s peripheral vision. The exam covers a range of over 130 degrees as this is required for some state licensing exams. The monocular version uses 100 positions ranging up to 70 degrees nasally, 50 degrees temporally, 30 degrees superiorly and 50 degrees inferiorly. The binocular version combines the monocular positions from both eyes for a total of 120 positions covering a 136 degree field of view.
The purpose of the Esterman lies in detecting any irregularities or deficiencies in the patient's visual field, which may indicate underlying eye conditions. For example, this test is particularly instrumental in diagnosing conditions such as glaucoma, retinal diseases, and optic nerve disorders. The grid's systematic approach aids in identifying specific patterns of visual field loss, contributing to accurate diagnoses and subsequent treatment plans.
How to Prepare a Patient for the Esterman Visual Field Test
Prior to administering the Esterman test, patient instructions and expectations play a crucial role in obtaining reliable results. Explain the test purpose, duration, and what to expect during the procedure. Inform patients to remain focused and respond promptly to light stimuli. Clear communication ensures that patients understand the importance of maintaining focus during the test, as well as the significance of accurate responses.
Healthcare professionals must also consider any necessary precautions or specific patient conditions that may affect the test results. For example, instruct patients to remove any contact lenses and wear glasses (if necessary), and consider potential cognitive or physical limitations that might affect their ability to understand or participate in the test. Addressing these factors beforehand helps streamline the testing process and ensures the reliability of the obtained data.
How to Perform the Esterman Visual Field Test (Step-by-Step)
The testing process involves the strategic use of the Esterman grid, a visual stimulus tool that systematically evaluates the patient's peripheral vision. The patient responds to the appearance of stimuli within the grid, enabling healthcare professionals to map the visual field and identify any anomalies or deficiencies.
The Esterman grid operates by presenting stimuli at varying intensities and locations, enabling a comprehensive assessment of the patient's peripheral visual field. This methodical approach ensures that no area of the patient's peripheral vision is overlooked, facilitating a thorough evaluation of their visual health.
Here is a general overview for conducting the Esterman Visual Field Test:
- Position the patient comfortably at the perimeter, ensuring proper headrest and chin rest placement.
- Explain the response mechanism (e.g., button press) and emphasize the importance of fixating on the central point throughout the test.
- Present light stimuli at various grid locations and record the patient's responses.
It’s important to note that this is just a general guideline, while the specifics of this exam may vary based on patient needs and technology capabilities. For example, if you are using a virtual visual field machine, the process may look a little different.
More comprehensive details on conducting visual field testing are offered by the American Academy of Ophthalmology (AAO). Additionally, several medical equipment manufacturers offer training materials and manuals specific to their perimeter models, which often include detailed instructions for the Esterman test.
Learn more about the Esterman test, and 20 other visual field and vision exams by downloading our Comprehensive Testing Guide.
Esterman Visual Field Test for Driving and DMV Requirements
The Esterman visual field test for driving is one of the most common functional visual assessments required by U.S. state DMVs and licensing boards. Because driving eligibility depends heavily on adequate peripheral vision, many states use the 120-degree visual field test, which is a standardized binocular assessment, to confirm that a patient meets the minimum horizontal field requirements.
Unlike traditional threshold tests, the Esterman exam evaluates functional, real-world vision, making it well-suited for determining whether visual impairments may impact a person’s ability to drive safely. For this reason, eye doctors frequently administer the Esterman to patients with glaucoma, retinal disease, neurological deficits, or post-stroke vision changes.
Driving Standards and Pass/Fail Criteria
Each state sets its own Esterman visual field driving standards, but a typical minimum includes:
- A horizontal binocular field of at least 120 degrees
- No dense central scotomas
- Acceptable sensitivity and reaction reliability
- A functional score consistent with safe peripheral awareness
Some state agencies also reference the Esterman Efficiency Score, a weighted measure of how many test points are seen and their importance within the driving field. Higher efficiency scores indicate stronger functional vision, while lower scores may trigger driving restrictions or further evaluation.
Why Eye Doctors Use the Esterman for Driving Evaluations
- Provides a real-world assessment of functional peripheral vision
- Fast, reliable, and broadly recognized across licensing bodies
- Captures binocular field loss that may not appear on monocular threshold tests
- Clearly documents functional vision for patients appealing driving suspensions or applying for reinstatement
How Virtual Field Supports DMV-Valid Esterman Testing
Virtual Field delivers clinically accurate binocular and monocular Esterman testing that aligns with DMV and state licensing requirements. Our portabie, lightweight headset improves patient compliance and produces consistent, high-quality results, making it easier for clinicians to document whether patients meet Esterman visual field driving standards and qualify for their 120-degree visual field test requirements.
For clinics that regularly perform driving evaluations, Virtual Field simplifies the testing process, enhances patient comfort, and provides fast, clear visual field maps and scoring.
Interpreting Esterman Test Results
Interpreting Esterman test results requires a nuanced understanding of the visual field patterns and a thorough examination of potential false positives and negatives. The significance of different patterns in the test results plays a crucial role in identifying specific eye conditions accurately.
Eye doctors should be adept at recognizing patterns indicative of conditions such as glaucoma, optic nerve disorders, and retinal diseases. Deviations from the expected norm in the Esterman grid should be carefully analyzed to determine the severity and extent of visual field loss, guiding appropriate treatment strategies.
Some commonly recognized patterns include:
- Arcuate Scotomas: These arcuate-shaped blind spots, typically nasal or temporal, are highly suggestive of glaucoma, especially when corresponding to the affected retinal nerve fiber layer.
- Central Scotomas: Dense central vision loss points towards macular pathologies like age-related macular degeneration or optic nerve issues.
- Stepwise Defects: These stair-stepped scotomas often indicate retinal vascular disease, such as diabetic retinopathy or branch retinal artery occlusion.
- Hemianopsia: Complete loss of vision in half the field (homonymous) suggests optic pathway lesions, while bitemporal hemianopsia can indicate pituitary tumors.
False Positives and Negatives
While the Esterman exam can be a valuable tool in eye care, it’s not 100% infallible. False positives and negatives are possible.
- False Positives: Fatigue, unreliable patient responses, media opacities, or improper testing technique can lead to missed stimuli, mimicking scotomas (blind spots). When the test indicates visual field defects that do not align with the actual condition, it can lead to unnecessary concern and intervention.
- False Negatives: Early glaucoma or subtle vision loss might go undetected with the Esterman's fixed-intensity stimuli. When the test fails to detect existing visual field abnormalities, it may result in overlooking critical pathology.
Eye doctors must meticulously evaluate potential confounding factors, patient education and cooperation, and the reliability of the testing environment to minimize the occurrence of false results, ensuring an accurate interpretation of the Esterman test and facilitating informed clinical decision-making.
Quantitative measures like mean deviation and Esterman Disability Score (EDS) provide additional insights, but clinical context remains paramount. Correlating Esterman findings with other tests (e.g., OCT, fundus exams) and patient history is crucial for accurate diagnosis and management. Remember, the Esterman test is a valuable tool, but interpretation demands expertise, pattern recognition, and awareness of limitations.
How to Interpret Esterman Visual Field Results (With Examples)
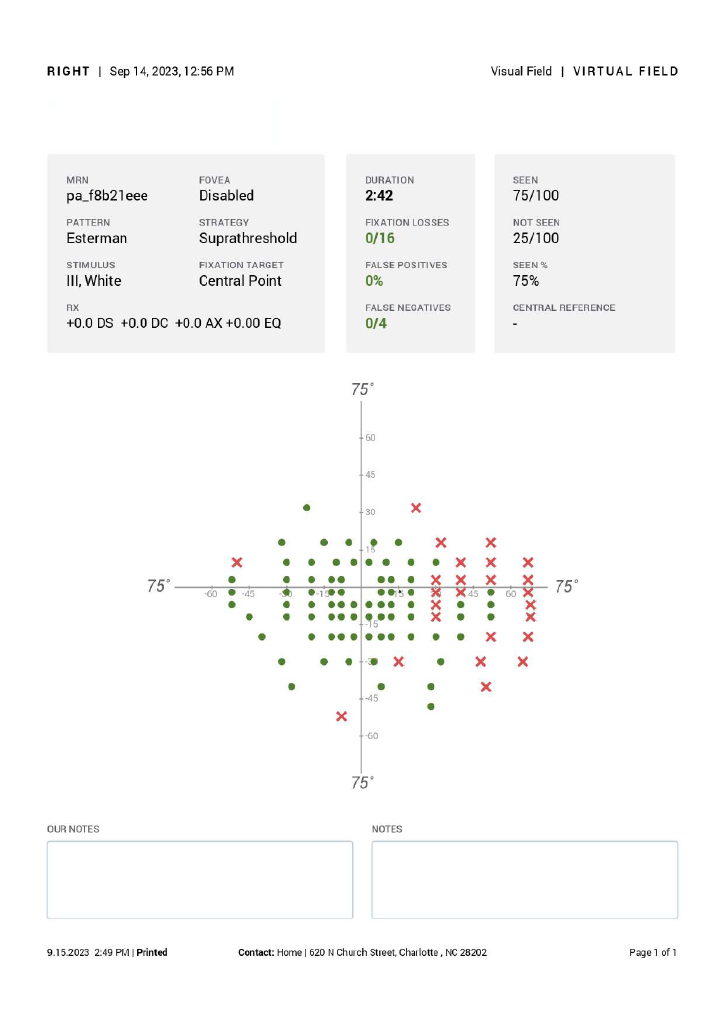
Accurate Esterman visual field interpretation requires understanding both the structure of the test and the clinical patterns that commonly appear in functional visual field loss. Unlike threshold-based examinations, the Esterman is a suprathreshold functional test, meaning that interpretation focuses on which points were seen, which were missed, and how those patterns relate to real-world vision tasks such as driving.
Key Principles of Esterman Interpretation
When learning how to interpret an Esterman visual field, clinicians should evaluate the following:
- Overall pattern of defects (central, arcuate, hemifield, or scattered)
- Consistency with known disease processes (e.g., glaucoma, optic neuropathy, retinal disease)
- Binocular vs. monocular differences
- Impact of defects on daily function, especially driving
- Reliability indicators, such as fixation losses or unusual response patterns
A normal Esterman visual field typically shows:
- Full peripheral detection across the 120-degree binocular field
- No dense central scotomas
- Minimal or no missed points in high-priority areas
- A smooth, symmetric pattern without abrupt step defects
This presentation generally indicates functional vision sufficient for daily activities and often meets the criteria for an Esterman visual field test pass in states that use the exam for DMV clearance.
Common Esterman Visual Field Patterns and What They Mean
1. Arcuate or Nasal Step Defects
Often linked to glaucoma, these defects appear as clusters of missed points forming a curved pattern.
Interpretation note: Compare with OCT RNFL to confirm correspondence.
2. Central or Paracentral Scotomas
Seen in optic nerve disease, macular pathology, or neurological conditions.
Interpretation note: Central involvement may impact driving clearance depending on the depth and location.
3. Hemifield or Quadrantanopic Loss
Frequently seen in optic tract lesions, strokes, and brain tumors.
Interpretation note: Even with adequate peripheral coverage, these patterns may disqualify patients from driving due to impaired awareness on one side.
4. Inferior Field Loss
Impacts mobility, fall risk, and obstacle detection.
Interpretation note: DMV standards vary, but inferior defects often have functional consequences.
Example Result Scenarios
Example 1: Normal Esterman
- 0–3 missed points
- No central involvement
- Full lateral expansion to approximately 120°
Interpretation: Normal functional vision. Likely qualifies for driving clearance.
Example 2: Moderate Glaucoma
- Missed points forming an arcuate scotoma
- Good central preservation
Interpretation: Functional impact depends on density and symmetry. May still meet some DMV standards.
Example 3: Homonymous Hemianopsia
- Complete loss on one side of the binocular field
Interpretation: Typically results in an Esterman visual field test pass failure for driving, though clinical explanations should be documented.
Using Virtual Field for Accurate Interpretation
Virtual Field provides clear, high-resolution Esterman output maps that make interpretation intuitive. By combining functional test results with OCT, fundus imaging, and patient history, clinicians can confidently perform accurate Esterman visual field interpretation and document results for clinical care or DMV requirements.
Conditions Diagnosed with Esterman Test
The Esterman visual field test is instrumental in diagnosing a spectrum of eye conditions such as glaucoma, optic nerve disorders, retinal diseases and other visual impairments. By pinpointing specific patterns of visual field loss, healthcare professionals can identify the presence and progression of these conditions, enabling timely intervention and management.
Glaucoma and Optic Nerve Disorders
The Esterman test plays a vital role in glaucoma diagnosis and management. By detecting characteristic peripheral vision loss patterns, it helps identify early-stage glaucoma and monitor disease progression. Similarly, optic nerve diseases like optic neuritis can show specific visual field defects detectable through the Esterman test.
Retinal Diseases and Visual Impairments
Retinal diseases can cause scotomas in specific areas of the visual field, often revealed by the Esterman test. Additionally, conditions like stroke or tumors affecting the visual pathway can manifest as visual field defects identified through this test.
Advantages and Limitations of the Esterman Visual Field Test
The Esterman visual field test stands as a valuable tool in the armamentarium of eye care professionals, offering a comprehensive assessment of peripheral vision. However, to use it effectively, it’s important to understand its pros and cons.
Advantages
The Esterman visual field test offers several advantages in the realm of eye care. Its comprehensive assessment of the visual field provides a detailed map of any irregularities, allowing for a more nuanced understanding of a patient's eye health.
Early detection and monitoring of eye conditions, such as glaucoma, enable timely intervention, potentially preventing irreversible damage and preserving the patient's vision. The Esterman test facilitates this by capturing subtle changes in peripheral vision.
What’s more, using virtual reality visual field testing can provide additional advantages by making the test more accessible to patients with limited mobility.
Limitations and Considerations
Despite its merits, the Esterman visual field test is not without limitations. The exam can be time-consuming and require patient cooperation, which might be challenging for children or individuals with cognitive limitations. Healthcare professionals must address the challenges associated with patient cooperation, potential learning effects, and the impact of fatigue during prolonged testing sessions.
Special cases or conditions, such as neurological disorders, may also affect the accuracy of the results, requiring careful consideration and additional diagnostic measures.
Additionally, the exam might not be sensitive enough to detect very subtle vision loss. False positives and negatives are possible, so it’s imperative that the healthcare provider pay special attention when interpreting results.
Why Virtual Field Is the Best Way to Perform the Esterman Visual Field Test
Performing the Esterman exam accurately and efficiently is essential—especially when results are used for DMV authorization, functional vision assessment, or clinical decision-making. Virtual Field streamlines this process by delivering a fast, comfortable, and clinically reliable way to conduct both monocular and binocular Esterman testing.
Key Advantages of Using Virtual Field for Esterman Testing
- Fully valid for U.S. DMV and 120-degree visual field requirements
- Supports both monocular and binocular Esterman tests
- Portable headset improves patient comfort and compliance
- Clinically validated suprathreshold algorithm ensures accurate functional mapping
- Faster testing with fewer fixation losses compared to traditional perimeters
Virtual Field helps eye care professionals perform efficient, patient-friendly Esterman exams while meeting the standards required for driving evaluations and clinical decision-making.
See how Virtual Field performs the Esterman test for DMV requirements — Get a Demo.
About Virtual Field
Virtual Field delivers an exceptional eye exam experience. Eye care professionals including ophthalmologists and optometrists examine patients faster, more efficiently, and more comfortably than ever before. Exams include Visual Field, 24-2, Kinetic Visual Field (Goldmann Perimetry), Ptosis, Esterman, Color Vision, Pupillometry, Extraocular Motility (EOM), and more.



